Ocular oncology, a specialized field at the intersection of ophthalmology and oncology, deals with the diagnosis and treatment of eye cancers—rare but potentially life-altering conditions that demand precision, urgency, and multidisciplinary care. 中環眼科中心 While the eye is a small organ, its complexity and proximity to the brain make ocular tumors uniquely challenging. From subtle symptoms to aggressive malignancies, navigating the landscape of eye cancers requires not only clinical expertise but also a deep understanding of the emotional and functional impact on patients.
Eye cancers can originate within the eye (intraocular), on its surface, or in surrounding structures such as the eyelids and orbit. Among the most common intraocular malignancies are uveal melanoma in adults and retinoblastoma in children. Each presents distinct diagnostic hurdles and therapeutic pathways, yet both underscore the importance of early detection and tailored treatment.
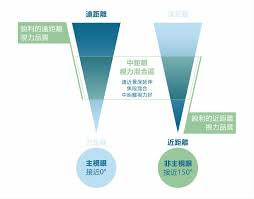
Uveal melanoma, the most prevalent primary intraocular cancer in adults, arises from melanocytes in the uveal tract, which includes the iris, ciliary body, and choroid. Unlike cutaneous melanoma, uveal melanoma is not typically linked to UV exposure, and its etiology remains partially understood. Patients may experience blurred vision, visual field defects, or photopsia, but many tumors are asymptomatic and discovered incidentally during routine eye exams. Diagnosis hinges on clinical examination, ultrasonography, and imaging modalities such as optical coherence tomography (OCT) and fluorescein angiography. Fine-needle aspiration biopsy may be employed for cytogenetic analysis, helping predict metastatic risk.
Treatment of uveal melanoma balances tumor control with vision preservation. Small to medium-sized tumors are often managed with plaque brachytherapy, a form of localized radiation that spares surrounding tissues. Larger or more aggressive tumors may necessitate enucleation—the surgical removal of the eye—to prevent metastasis. Despite successful local treatment, uveal melanoma carries a significant risk of liver metastases, prompting ongoing surveillance and, in some cases, systemic therapy. Advances in immunotherapy and targeted treatments are being explored, though their efficacy in ocular melanoma remains under investigation.
In contrast, retinoblastoma is a pediatric cancer that typically presents before the age of five. It originates from retinal cells and is often hereditary, linked to mutations in the RB1 gene. The hallmark sign—leukocoria or “white pupil”—is frequently noticed by parents in photographs or dim lighting. Strabismus, eye redness, and vision loss may also occur. Diagnosis involves a detailed fundus examination under anesthesia, along with imaging studies such as MRI to assess extent and rule out intracranial involvement.
Retinoblastoma treatment has evolved dramatically over the past decades. Historically, enucleation was the primary approach, but today, eye-sparing therapies are prioritized when feasible. Systemic chemotherapy, intra-arterial chemotherapy (delivered directly to the ophthalmic artery), and intravitreal injections are used to shrink tumors and control vitreous seeds. Focal therapies like laser photocoagulation and cryotherapy complement systemic treatment. The goal is not only to save the eye but also to preserve vision and minimize long-term side effects. Genetic counseling and screening of family members are integral, given the hereditary nature of the disease.
Beyond intraocular cancers, ocular oncology also addresses tumors of the eyelid, conjunctiva, and orbit. Basal cell carcinoma is the most common eyelid malignancy, often linked to sun exposure. Though slow-growing, it can invade surrounding tissues and compromise ocular function. Surgical excision with margin control is the standard treatment, sometimes requiring reconstructive procedures to restore eyelid anatomy. Squamous cell carcinoma and sebaceous gland carcinoma, though less common, tend to be more aggressive and may necessitate wider excision or adjunctive therapies.
Conjunctival tumors, including melanoma and lymphoma, pose diagnostic challenges due to their subtle appearance and mimicry of benign lesions. Biopsy is essential for accurate diagnosis, and treatment may involve excision, cryotherapy, topical chemotherapy agents like mitomycin C, or radiation. Orbital tumors, which arise behind the eye, can cause proptosis, pain, or vision changes. Imaging with CT or MRI is crucial for localization, and management depends on tumor type—ranging from surgical debulking to systemic chemotherapy or radiotherapy.
The psychological toll of eye cancers cannot be overstated. Vision is deeply tied to identity, independence, and quality of life. The prospect of losing an eye or experiencing visual impairment evokes profound fear and grief. Ocular oncologists must navigate not only the medical complexities but also the emotional terrain, offering compassionate care and clear communication. Support groups, counseling, and rehabilitation services play a vital role in helping patients and families cope with diagnosis and treatment.
Technological innovation continues to reshape ocular oncology. Artificial intelligence is being harnessed to analyze retinal images and detect subtle changes indicative of malignancy. Molecular profiling of tumors allows for personalized treatment strategies, targeting specific genetic mutations. Minimally invasive surgical techniques and precision radiation delivery are improving outcomes while reducing complications. Telemedicine is expanding access to specialized care, particularly in regions where ocular oncology expertise is scarce.
Despite these advances, challenges remain. Eye cancers are rare, and many clinicians may encounter only a handful of cases in their careers. This rarity can lead to delayed diagnosis or mismanagement. Raising awareness among healthcare providers and the public is essential for early detection. Research funding is also limited compared to more common cancers, underscoring the need for advocacy and investment in ocular oncology.
Collaboration is the cornerstone of effective eye cancer care. Multidisciplinary teams—including ophthalmologists, oncologists, radiologists, pathologists, and genetic counselors—must work in concert to deliver comprehensive treatment. Institutions with dedicated ocular oncology centers offer the best outcomes, combining clinical expertise with cutting-edge research and holistic support.
In the end, ocular oncology is not just about preserving sight—it’s about preserving life, dignity, and hope. Each patient’s journey is unique, shaped by the type of cancer, the treatment path, and the personal meaning of vision. As science advances and awareness grows, the future of ocular oncology holds promise: earlier detection, more effective therapies, and a deeper understanding of the human experience behind every diagnosis.